Health insurance claim process: the greatest steps
A health insurance policy kicks in when the insured is admitted to the hospital or when they experience a medical emergency and have to pay for it. A health insurance claim is stated to have happened at that point if the hospitalization or the medical costs were paid by the health insurance plan. In the case of health insurance claim process: the greatest steps, the insurance provider will cover any medical costs that arise. Let’s explore with topfoodss.com!.
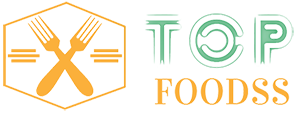
What are the Health insurance claim process Steps?
Although they resemble billing statements, medical claims are slightly more detailed. To get paid for medical services, healthcare professionals submit health insurance claim process firms. These claims make sure that private insurance companies pay providers in addition to the coinsurance that employers and workers each contribute as a proportion of the cost of a service.
Even while you might be aware of the process for submitting medical claims to a private insurance provider, you might not be familiar with it. Unnecessarily complex claim processing procedures used by traditional health insurance claim process, however, allow for a relatively significant margin of error.
Although different insurance companies may somewhat alter the procedure, they all typically follow a similar foundation. Here are the most typical procedures in the health insurance claim process so that readers may comprehend this complicated system, including:
File claim. A claim must be submitted in the form of a physical document or electronically as the initial step in the health insurance claim process procedure. A claim filed in hard copy form has to be converted to digital form.
Initial review. The insurance company examines the claim after receiving it to make sure it was submitted during the correct window of time. A software program often looks for duplicate charges or false data as well.
Verify member. The health insurance claim process provider checks their system to determine if the member has an active insurance plan in order to confirm the member’s eligibility.
Verify network. The insurance company verifies that a member provider in their healthcare network provided the services listed on the claim.
Apply negotiated price. With providers in their networks, insurance firms have agreements that set fixed-price discounts. Once the member and network have been validated, these agreed-upon prices are applied.
Verify member benefits. The health insurance claim process verification of membership information, including whether the member’s benefits cover the services, which benefits apply where, and what portion of cost-sharing the member and their employer are liable for paying, is one of the longest phases of the procedure.
Verify medical necessity. The insurance provider determines if the treatments indicated on the claim are required for the patient’s medical requirements after verifying the member, network, and benefits.
Evaluate claim risk. Software used by the firm automatically detects claims that may include insurance fraud.
Issue payment to provider. The insurance company pays the provider after verifying the legitimacy of the claim.
The (EOB) Communicate Explanation of Benefits to members. Members receive an EOB statement—not a bill—that lists the entire cost of the services provided, the amount their insurance will cover, and the coinsurance they will be responsible for.
Bill patients and employers for the remainder. The patient and the employer are liable for paying the costs if treatments are rendered that the insurance does not cover. They receive a bill from the provider, which often matches the EOB.
Types of Health insurance claim process
Typically, one of the following methods can be used to submit a claim:
Cashless health insurance:As the name implies, while making a claim on cashless health insurance, you are not required to pay the whole hospital charge. When you use a cashless mediclaim, you do not need to keep track of the bills and other invoices for submissions. Simply keep your Cashless Health Card on hand. Keep in mind that only network hospitals are permitted to accept cashless medical claims. A network hospital is one that your health insurance provider has a relationship with. Your insurance company will be able to pay the hospital directly in this way. A cashless claim is not entirely cashless; you must instead offset deductibles with a small sum of money.
Reimbursement Claims: You have the option to receive care at any hospital of your choosing or convenience. A network hospital is not required. You must first pay for the total cost of the therapy in this form of claim, gather all relevant receipts and other documentation, and then submit a reimbursement claim. Your health insurance provider will pay the claim amount after deducting the deductible after your claim is accepted.

Conclusion
Even though there are many considerations to ponder when selecting a health insurance plan, it is always preferable to be safe than sorry. And in the post-pandemic era, where we frequently face unforeseen occurrences, this has shown to be especially true.
The greatest way to protect your wealth and guarantee that you have enough money to get the best care is to invest in a health insurance coverage. This will benefit both your short- and long-term financial health. Make careful to select the greatest health insurance claim process plan in accordance with your needs and those of your family.